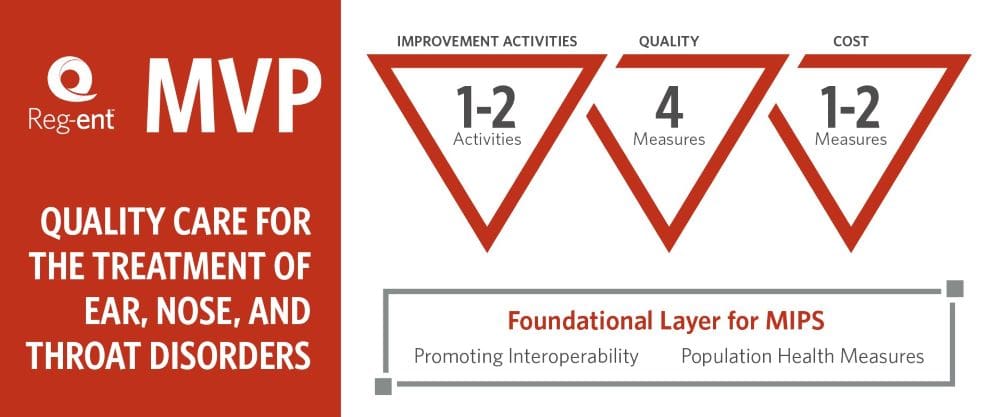
About Otolaryngology MVP (MIPS Value Pathways)
MVPs are the newest MIPS reporting option (an alternative to traditional MIPS and APM Performance Pathway (APP)) that you can use to meet your MIPS reporting requirements. Each MVP includes a subset of measures and activities that are related to a given specialty or medical condition. CMS has indicated their intent to sunset traditional MIPS but not officially announced the change through rulemaking.
The Reg-ent team at the AAO-HNSF has codeveloped with CMS the MIPS Value Pathway focused on Otolaryngology, “Quality Care for Ear, Nose, and Throat” which was finalized as an approved MVP as outlined in the 2024 Medicare Physician Fee Schedule Final Rule. The MVP focuses on caring for patients experiencing some of the most common otolaryngology conditions such as otologic conditions, chronic rhinosinusitis (CRS), age-related hearing loss (ARHL) and otitis media. This MVP would be most applicable to Otolaryngologists and applicable Non-Physician Practitioner (NPPs) such as audiologists , nurse practitioners, and physician assistants.
What is the difference between traditional MIPS and MVPs?
| Traditional MIPS | MIPS Value Pathways |
| Four performance categories leveraging the entire measure and activity inventory for Quality, Promoting Interoperability, Improvement Activities and Cost. | Subset of quality and cost measures and improvement activities are specific to a given specialty or medical condition. |
| For the Quality performance category, 6 measures are required for reporting from a broad selection of quality measures. | For the Quality performance category, 4 measures are required to be reported with additional population health measures calculated by administrative claims. |
| Does not allow subgroup reporting | Allows subgroup reporting |
| Allows clinicians to opt-in or voluntarily report | For Improvement Activities, credit is provided and point value doubles for MVP participation. |
| Foundational layer consists of administrative claims quality measures and Promoting Interoperability | |
| Does not allow clinicians to opt-in or voluntarily report |
What measures are included in the Otolaryngology MVP?
Please note, quality measures with the ‘AAO’ prefix are only available to Reg-ent participants. Per CMS policy, Qualified Clinical Data Registries (QCDRs) and QCDRs with permission from the measure steward can submit QCDR measures. Qualified Registries (QRs) and EHRs are limited to the MIPS quality measures.
| Measure ID | Measure Title |
|---|---|
| AAO20 | Tympanostomy Tubes: Comprehensive Audiometric Evaluation |
| AAO21 | Otitis Media with Effusion (OME): Comprehensive Audiometric Evaluation for Chronic OME > or = 3 months |
| QPP128 | Preventive Care and Screening: Body Mass Index (BMI) Screening and Follow-Up Plan |
| QPP226* | Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention |
| QPP277 | Sleep Apnea: Severity Assessment at Initial Diagnosis |
| QPP331 | Adult Sinusitis: Antibiotic Prescribed for Acute Viral Sinusitis (Overuse) |
| QPP332 | Adult Sinusitis: Appropriate Choice of Antibiotic: Amoxicillin with or Without Clavulanate Prescribed for Patients with Acute Bacterial Sinusitis (Appropriate Use) |
| QPP355 | Unplanned Reoperation within the 30-Day Postoperative Period |
| QPP357 | Surgical Site Infection (SSI) |
| QPP487* | Screening for Social Drivers of Health |
Note: Measure IDs with (*) denotes measures applicable for Audiologists.
Which is the right reporting option for my practice?
- Reg-ent participants are encouraged to work on the early adoption and implementation of using a limited number of quality measures available in the MVP to allow clinicians to get comfortable with reporting to CMS via MVPs and prepare for any potential practice workflow changes.
- To report MVP for 2025, we recommend suing the following checklist:
- Confirm your eligibility. Voluntary reporters, opt-in eligible clinicians, and virtual groups can’t report an MVP for the 2025 performance year.
- Selecting Quality measures: Evaluate the scoring potential for at least 4 quality measures within the MVP or 6 applicable quality measures for traditional MIPS.
- Confirm which improvement activities would fulfill the requirements.
- Review the population health measure criteria: The population health measure will be scored as part of the quality performance category. If your selected population health measure does not meet the case minimum measure requirements or the measure does not have a benchmark it will be excluded from scoring.
- Confirm if you are a part of a multispecialty group: beginning in performance year 2026, multispecialty groups will be required to form subgroups to report MVPs.
- Ask a Reg-ent team member to assess your score using the Reg-ent Scoring Wizard to see how last year’s performance will score in 2025. This will estimate a potential score for both traditional MIPS and MVPs.
Frequently Asked Questions
1. Who will MVPs impact?
Any MIPS eligible clinician, group, virtual group, or opt-in participant will be impacted by the transition.
2. When are MVPs being implemented?
Over the next few years, CMS intends to sunset traditional MIPS. Initially, their intent was to complete the transition in 2027. This has not been officially proposed.
3. Am I required to report MVPs?
MVPs are one option for meeting your MIPS reporting requirements beginning with the 2023 MIPS performance year. You can also meet MIPS reporting requirements through traditional MIPS and the APM Performance Pathway (APP), though CMS intends to sunset traditional MIPS through future rulemaking.
4. When should my practice make the transition from traditional MIPS to MVPs?
As traditional MIPS is phased out, practices should look at the quality measures included in an applicable MVP and begin mapping and refining the MVP measures while traditional MIPS is still available. Being prepared for the limited subset of measures will allow time to implement quality initiatives or clinical workflows before being scored on the metric.
5. Why is CMS sunsetting traditional MIPS and moving toward MVPs?
CMS’s intent is to provide a more cohesive participation experience, reduce burden and complexity, and include measures that are meaningful and applicable to each specialty. Their hope in limiting the choice of measures will result in scoring similar data sets across the specialty. In addition, their goal is to standardize the measures within MVPs to produce data that can better assist patients in comparing clinician performance and selecting clinicians from which to seek care.
6. How and when should we register for MVPs?
You can register for an MVP during the MVP Registration Window of April 1 – December 1, 2025. You can refer to CMS 2025 MVP Registration User Guide that will describe how you can register to report an MVP for the 2025 performance year.
7. Can a clinician report multiple MVPs?
A clinician can participate in multiple ways to report multiple MVPs. A clinician can participate as an individual, subgroup, group, APM Entity, or in any combination of these 4 participation options.
8. Are there any flexibilities available to small practices that wish to report an MVP?
Small practices will continue to have flexibility when reporting an MVP, just as in traditional MIPS such as receiving bonus points and automatic re-weighting of the Promoting Interoperability performance category.
9. How does MVP affect my performance feedback?
Similar to traditional MIPS, clinicians will receive the final performance feedback and payment adjustment in July- August reflecting the highest final score that could be attributed to your TIN/NPI combination. For MVP submission, in addition to your final score and payment adjustment MVP participants will also receive “MVP Comparative Feedback” during this phase. MVP comparative feedback will highlight how your performance compares at the category level to other clinicians reporting the same MVP.